- India
- International
‘None of the scientists forecast second wave of such vehemence’
"The ferocity of the second wave did take everyone by surprise. During the first wave, multiple measures were initiated for revamping response infrastructure." says K Vijay Raghavan, Principal Scientific Advisor to the Union government.
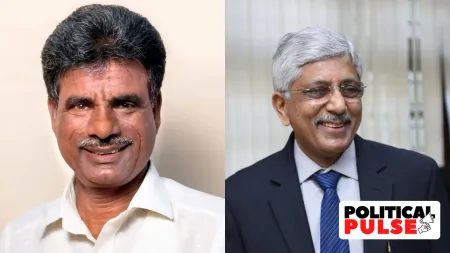
 K Vijay Raghavan, Principal Scientific Advisor to the Union government
K Vijay Raghavan, Principal Scientific Advisor to the Union governmentAmidst continuously rising coronavirus numbers in India, Principal Scientific Advisor K VijayRaghavan spoke to Amitabh Sinha on what went wrong, why there couldn’t be enough infrastructure for a surge like this, and whether there was any end in sight.
Were we taken by surprise by the ferocity of the second wave? Why? What was the worst case scenario that we had prepared for after the first wave, and how different is this from what we had prepared for?
The ferocity of the second wave took everyone by surprise. Prior to the first wave, the predictions were dire. The response to those predictions was electric and everyone came on board from the start to address an unknown. The relatively lower severity in India during the first wave and the squelching of that wave have been discussed widely. Lockdowns, ensuring physical distancing, adoption of masks, and the extraordinary and rapid action from our health services all contributed, and had a strong impact. During and after the first wave, multiple measures were initiated by the Centre and states for revamping response infrastructure. This, and the flattening of the first wave, and the confidence from vaccine development all contributed to us not anticipating the size of this surge. There were other important reasons too.
We had seropositivity results from tests conducted in some metros, which suggested that we had a pool of recovered, possibly immune, people that would help in bending the curve. The seropositivity tests were well done, but their results should not have been taken as the average for the entire large metros. Some people did.
Also, we had just weathered the first wave, and scientists, both within and outside the country, were anticipating that the second wave would be of similar size or lower. None of the national or global experts, including those at IHME (Institute of Health Metrics and Evaluation at the University of Washington) or LANL (Los Almos National Laboratory in the United States), were forecasting second wave of such vehemence. In fact, many indeed put it (the intensity of the second wave) explicitly lower than the first wave under conditions then present.

The reasons for the extraordinary intensity of the second wave are still being looked into. But, three factors are likely to be at play — public behaviour, increased susceptibility of the population, and new variants of the virus. The greater-than-expected susceptibility may simply be a reflection of the heterogeneity in the exposure to the virus during the first wave. Certain sections of the population were more exposed than others during the first wave, but in the second wave, newer sections were exposed. Or, the greater susceptibility could also be linked to the emergence of new variants.
 Covid patient talks over the phone during their long wait inside an Ambulance at Civil Hospital in Asarwa on Wednesday.
Covid patient talks over the phone during their long wait inside an Ambulance at Civil Hospital in Asarwa on Wednesday.
Data from one survey in February showed some decline in neutralizing antibodies in the previously infected people, despite persistent seropositivity. So, diminishing immunity could also be a factor, though many other studies also show that even eight months after infection, about 80 per cent immunity still remained.
Many factors could be contributing to the intensity of the second wave, each by small extents, but, together, these are resulting in very large impact in a situation where the growth is exponential.
Based on serological extrapolations, we were fully aware that the low symptoms and mortality in the first wave were, at least in part, due to the young age and possibly different exposure histories of the strata most affected. But, we perhaps mentally generalized it to others who had protected themselves well in the first wave, and were exposed now.
How would you respond to the criticism that we failed to anticipate the crisis? In fact, we actually became complacent when we got a breather, when all the scientists and health experts were warning against the second wave (no one could have predicted the timing or intensity, of course). Why have we been behind the curve? Did we drop our guards?
Indeed, health experts within and outside had been warning us about the second wave. While we were all aware of second waves in other countries, we now had vaccines at hand, and as mentioned earlier, no indications from serosurveys suggested the scale of the surge that what we are seeing. The variants, already known, were indeed a concern. So, it became a race to vaccinate as many as we could, while also maintaining Covid- appropriate behaviour. These were the only tools we had. Doing the former (vaccinating everyone) takes time. We slackened on the latter (following Covid-appropriate behaviour). Indeed, an analysis of publicly available mobility data of smartphones shows an very large increase in movement of people in the months just preceding the second wave. This, and poor masking could have had important effects.
Many components contribute to the value of R-nought, which tells us how infectious the disease is. A very small increase or decrease in the value of each component that contributes to R-nought can make a very big difference in its effect during an exponential growth. Thus, exposure of population previously uninfected, and protected, waning immunity, lax public behaviour, at individual level, as well as large crowds and gathering, emergence of new variants, each contribute in a negative way (to an increase in R-nought). No one factor needs to be the dominant one. Together, they are devastating. It is not easy for us to appreciate the power of the exponential and each contributor can feel they have contributed very little to the rise.
 Relatives mourn the death of a Covid patient outside Civil Hospital in Asarwa, Ahmedabad.
Relatives mourn the death of a Covid patient outside Civil Hospital in Asarwa, Ahmedabad.
The importance of following precautions and getting vaccinated to prevent second waves was emphasized repeatedly. There was perhaps a numbing in signalling and response. From late January 2021 onwards, in innumerable TV and media discussions and briefings on the vaccine rollout, everyone had been emphasising that until most are vaccinated, we must follow Covid- appropriate behaviour. Perhaps we got used to hearing this too often. It is not easy to be observant for so long, but this is literally a matter of life and death.
At the same time, people were also exposed to pseudo-science and misinformation. Some of this was coming from sources that the general public could safely assume to be credible, such as ones promoting ‘herd-immunity’ by allowing and modestly calibrating disease spread . That led to a confusion in messaging, and impacted public behaviour.
Further, the new variants are also possibly contributing significantly to the increased susceptibility. Unless this increase is matched by increased changes in factors which decrease the spread, we put ourselves in a situation of escalation instead of keeping cases low.
There were major efforts by central and state governments in ramping up hospital and health care infrastructure during the first wave. That wave gave us many tools and understanding on what to do at the hospital end. But, as that wave declined, so perhaps did the sense of urgency to get this completed.
However, two very important points must be kept in mind. It is just not possible to amplify the capacities of a public health system within a year to a level that would be sufficient to cope with what we are seeing now. If the requirements were in the same range as in the first wave, it could have been handled. You can build about 20-50 per cent more capacity in one year in some locations. Even there, lack of personnel will soon debilitate the response even if infrastructure is ramped up. A five-fold increase in capacity cannot be built in a year. Other measures to respond to such situations and/or prevent them must be considered in future.
Should there be a third wave, would we be able to handle it more effectively?
The long-term way of dealing with a crisis like this is not to create permanent vast excess capacities that will be adequate for a five-fold or ten-fold rise in cases. The important thing is to broaden and strengthen our baseline capacities, and, at the same time, prepare auxiliary capacities that can be pulled in during times of crisis. We need a large number of people with awareness and basic training, who can be in a position to contribute in emergencies. One can probably look for parallels like the territorial army or NCC in the area of defence. In a national crisis, everyone should be able to contribute. But they have to be prepared for a role.
We are still in fire-fighting mode, but is something already being done for a long-term on these lines?
Yes, certainly. We are already on our way. That is why I am telling you this.
With the benefit of hindsight, what are the three or four things that we could have done differently that would have placed us in a slightly better situation right now?
Not differently, but more rigorously perhaps. Measures like widespread use of masks and restrictions on large public gatherings should have been more strictly enforced, and abided by. Molecular, and public health, surveillance could have been better integrated. These things are applicable even today.
We need to strengthen our healthcare infrastructure, especially provisions for oxygen, ramp up training of personnel who can be summoned for emergency duty.
 A Covid-19 patient from Yerwada waiting for admission in a school van with oxygen outside Jumbo Covid centre at Shivaji nagar, Pune.
A Covid-19 patient from Yerwada waiting for admission in a school van with oxygen outside Jumbo Covid centre at Shivaji nagar, Pune.
Again given the level of this current surge, the impact of such measures would have been high only if stringent Covid-appropriate behaviour, and scaled-up testing and isolation was rigorously practised from the start. In our diverse contexts, this did not happen. It is not very easy to practice or enforce. A rapid overload of the health-care system to very difficult levels has thus taken place. This has happened in other countries too. Preventive measures are key to ensure that overloads do not happen. We must do everything we can to bolster health support now. It is already being done. But even going ahead in this wave, there is no escape from rigorously practising physical distancing in tried and innovative ways.
What is our current understanding of the main reasons for the ferocity of the second wave? How good is the evidence that it has been caused by a faster-transmitting mutant (the double mutant, or anything else)?
There is evidence for faster transmitting variants contributing to the surge. B.1.1.7 (the UK variant), with known higher transmissibility, is driving outbreaks in North India, reaching nearly 100 per cent levels in Punjab and about half or more in Delhi, Haryana, and UP. Its prevalence is rising in Rajasthan and Kerala as well. B.1.617 (the double mutant as it is commonly referred to) was associated with outbreaks in Maharashtra, where transmissibility increased after its appearance. This variant is increasing in Delhi, and Bengaluru, along with B.1.1.7. Evidence suggests that both these variants have similar transmissibility. For example, left unmitigated, B 1.1.7 will increase R-nought exponent by about 40 per cent, adding around 0.8 to an R-nought of 2. Mitigation, through face masks and physical distancing is key.
It is public knowledge that the double mutant was first noticed in October last year. It has been over six months now. We are still not sure whether or not the second wave can be (mainly) attributed to this mutant. Why should it take us so much time to ascertain this?
It is incorrect to say that it was noticed in October in India. The October sequences are recently deposited, and are either wrongly timestamped or deposited late. The earliest sequences deposited, that were available in March 2021, were from December 7. This was when the epidemic was in a declining phase in India. L452R (one of the two key mutations in the double mutant) had not yet been reported from California as an important mutation. There would have been no reason to flag the variant as important at that time.
The double mutant was identified by epidemiologic correlation of the sequencing data from Maharashtra from February 2021, with the data from California published between end January and early February 2021. The note to the Health Ministry was sent in early March 2021, identifying it as a Variant of Interest. This could not have been much faster.
Why have we been slow in gene sequencing efforts? How has it hampered our response?
Gene sequencing for COVID surveillance is not just about the sequencing exercise itself. There are lots of moving parts and logistics involved between sample collection at the districts, and gene sequencing in the laboratories. National health agencies have the networks and personnel, but lack the basic-science insight into the importance and urgency of such an exercise in a rapidly evolving pandemic-like situation. Laboratories have the skills and infrastructure to carry out sequencing but do not have the networks required for sample collection, storage and transportation. This gap was bridged in December and INSACOG (Indian SARS-CoV-2 Consortium on Genomics) was formally created in January 2021. Sequencing has picked up since then.
A lot of scientists have complained of lack of adequate data, from testing, serosurveys or gene sequencing. What have been our constraints, and again, how has this hampered our response.
In normal situations, speed is not usually critical, quality is. Laboratories discuss, verify and release information in due course. In an emergency situation, when speed and correctness are both needed, we can either be fast, and be open to multiple narratives from various eyes with inaccuracies corrected post facto, or be careful, with accurate but delayed summarized results that have passed multiple eyes.
In the first option, there is a possibility of downside confusion of multiple messages on early data. In the second, a sense of opacity can be perceived, and there could be complaints by those who would like to contribute to make things better.
The ministries and science laboratories are speeding up cycles of science communication, while maintaining accuracy. A balanced mechanism is there and feedback for improvement is always welcome.
Did we miscalculate on the vaccine front? Both Serum and Bharat Biotech were supposed to have increased their capacities. It hasn’t happened, though both of them have said it will happen soon. Was Serum expecting some monetary help from the government to set up new facilities? Should we have tried to access more vaccines upfront (something like the US or UK did)?
Increasing production capacity is not a singular activity. It needs to be accompanied by a corresponding increase in the abilities to ensure quality checks and testing, ability to transport and distribute. What can be done well on one scale sometimes is not readily scale-able to the next without careful testing again. Increasing capacity also requires more people. Manufacturing capacity can only double slowly, while the disease doubling time is very fast. That is why each question, on the speed of vaccine roll-out, or other logistics, ends almost with a ritual non sequitur: “Yes, this is what is being done, but in the meanwhile, follow Covid-appropriate behaviour.” This is not to blame people or abdicate responsibility. It will take time to vaccinate all. Till then, help in every way on the immediate tasks, and practice physical distancing the best you can.
Also, the model adopted by the United States or other countries in procuring vaccines may not be the most effective or useful for us. Look at the kind of money that was poured into Operation Warpspeed (of the United States), for example. Not every country has that kind of money. Also, that money was not all meant only for procurement of vaccines. It was not just to cover the costs of the companies but was also some sort of stimulus. It may have be disproportionate to the specific need for procuring vaccines.
 Covid patient with oxygen support waits to get admission at the 600-bed Covid ward at Civil hospital in Gujarat’s Gandhinagar.
Covid patient with oxygen support waits to get admission at the 600-bed Covid ward at Civil hospital in Gujarat’s Gandhinagar.
Yet, that does not mean that India became totally dependent on two vaccines or two companies only. We have arrangements to bring in more vaccines, and they would be coming in the next few months. Serum has an arrangement with Novavax. This will come by about July. Johnson & Johnson has tied up with Biological E. This will come soon. Zydus should be ready in some time. Sputnik is already there. All of this has been facilitated actively from early last year, at the start of the pandemic. That is why we can have them now and soon.
The intensity of the second wave has made everything look stressed. But on the vaccine front we are ramping up fast. Meanwhile, we should mask up and stay safe.
As the principal scientific advisor, what has frustrated you the most (lack of coordination, shortage of resources, flow of misinformation, or anything else)? What, according to you, has been the biggest constraint on our response?
We are dealing with a crisis of unprecedented proportions. But we have seen enormous effort being put in by everyone — common people, NGOs, local government, state governments, central government. Most important is the heavy lifting done by people in the health sector. The suffering we see and the pain being endured is heart-rending.
Difficulties in getting things done in a crisis like this are par for the course. That should not be conflated with frustration. No matter what the situation, we all have to work our way out, and we know what will help. Let us work to get things done, help each other and do both with humility and compassion. This is a tough time and we can get out of this. There is no time for frustration or giving up , and no one is giving up, across the spectrum.
Resources and supply chains are, of course, fully stretched, given the intensity of the surge. Information has to compete with misinformation which has no restraint and travels faster. It is agonizing what our people are going through and everyone at every level is working to change this. Ensuring that we get out of this is a shared task before us all.
Do you think we failed to effectively counter misinformation being spread through media, including social media? How has it hampered our response?
Effectiveness of communication on facts, vaccines and behaviour is very important. In today’s world this will be a never-ending task, and one always needs to look at impact and act accordingly. Information is often nuanced and calibrated and amplifies slowly. Misinformation is unbridled and spreads virally. We must constantly address this problem.
 Health workers wearing personal protective equipment (PPE) carry wood to prepare a funeral pyre for a coronavirus disease (COVID-19) victim during a mass cremation at a crematorium in New Delhi, India, April 26, 2021. (Image: REUTERS)
Health workers wearing personal protective equipment (PPE) carry wood to prepare a funeral pyre for a coronavirus disease (COVID-19) victim during a mass cremation at a crematorium in New Delhi, India, April 26, 2021. (Image: REUTERS)
Based on the inputs that you would have, when is the curve likely to begin to bend? Which are the states of concern?
Maharashtra may have reached a plateau, but the next few days will tell better. In Delhi, hopefully, we will start seeing a decline soon. India may peak in May, but much depends on what we do by way of behaviour.
We have to be careful about reaching conclusions from day to day decline in numbers. The situation in Uttar Pradesh continues to be a concern. Also, in Tamil Nadu and Karnataka.
West Bengal, Bihar and Jharkhand also need to be extremely watchful. All these states, by the way, can still turn around things. It is not that the situation has to deteriorate further. With immediate strong action, it is possible to prevent further deterioration.
We must prevent hospitals from being overwhelmed in new locations where increases are likely. For this, further and quick strengthening of infrastructure, oxygen supply, deployment of additional personnel, and behaviour-change are key. I cannot emphasise this enough but masks and physical distancing is absolutely crucial. The magnitude of infections we are seeing could lead to a more compressed course on the time-scale. This could mean faster rises, faster declines, and long, perhaps fat, tails of decline.
Ensuring continued surveillance, behaviour change and vaccination-expansion during the long tail phase is critical to prevent a third phase. We all know what to do and if we each do it relentlessly we can get out of this sooner rather than later.
Apr 24: Latest News
- 01
- 02
- 03
- 04
- 05